This is an invited submission for Healio.com, an online resource for doctors and surgeons published by SLACK Incorporated. Dr. Devgan has been invited to contribute on issues related to skin care, aging, and cosmetic surgery. This piece is intended for a professional medical audience. For additional information about making your eyes look younger, eye creams, tear trough fillers, or eye lift surgery, please contact our office at 212.452.2400 or info@LaraDevganMD.com.
Rejuvenating Your Eyes: A Plastic Surgeon's Approach
By Lara Devgan, MD, MPH
The skin around the eyes is the thinnest on the body, and consequently, it is the first place where your age is revealed. Among aging starlets and society doyennes alike, the periorbita is a shibboleth-- no matter how well-styled you are, there is no hiding from the sun damage, saggy skin, and volume loss around your eyes.
The market is flooded with a host of topical treatments. Indeed, skin care and cosmeceuticals devoted to the facial skin have become a billion dollar industry. Although topical treatment alone is not sufficient for more extensive periorbital aging, it is a good place to start for younger patients.
By the early 30s, men and women who are concerned with facial and periorbital aging should be using a skin care regimen that includes a retinoid, a vitamin C, and a sunscreen. Retinoids are key in increasing cell turnover and polishing away the appearance of fine lines. Vitamin C decreases free radical damage and brightens skin. Sunscreen helps prevent ongoing damage from taking place.
By the 40s or 50s, most men and women have periorbital aging that cannot be controlled with skin treatments alone. The upper lid skin droops, the lower lid fat pads bulge out, extra skin appears crepey, and dark circles become more prominent.
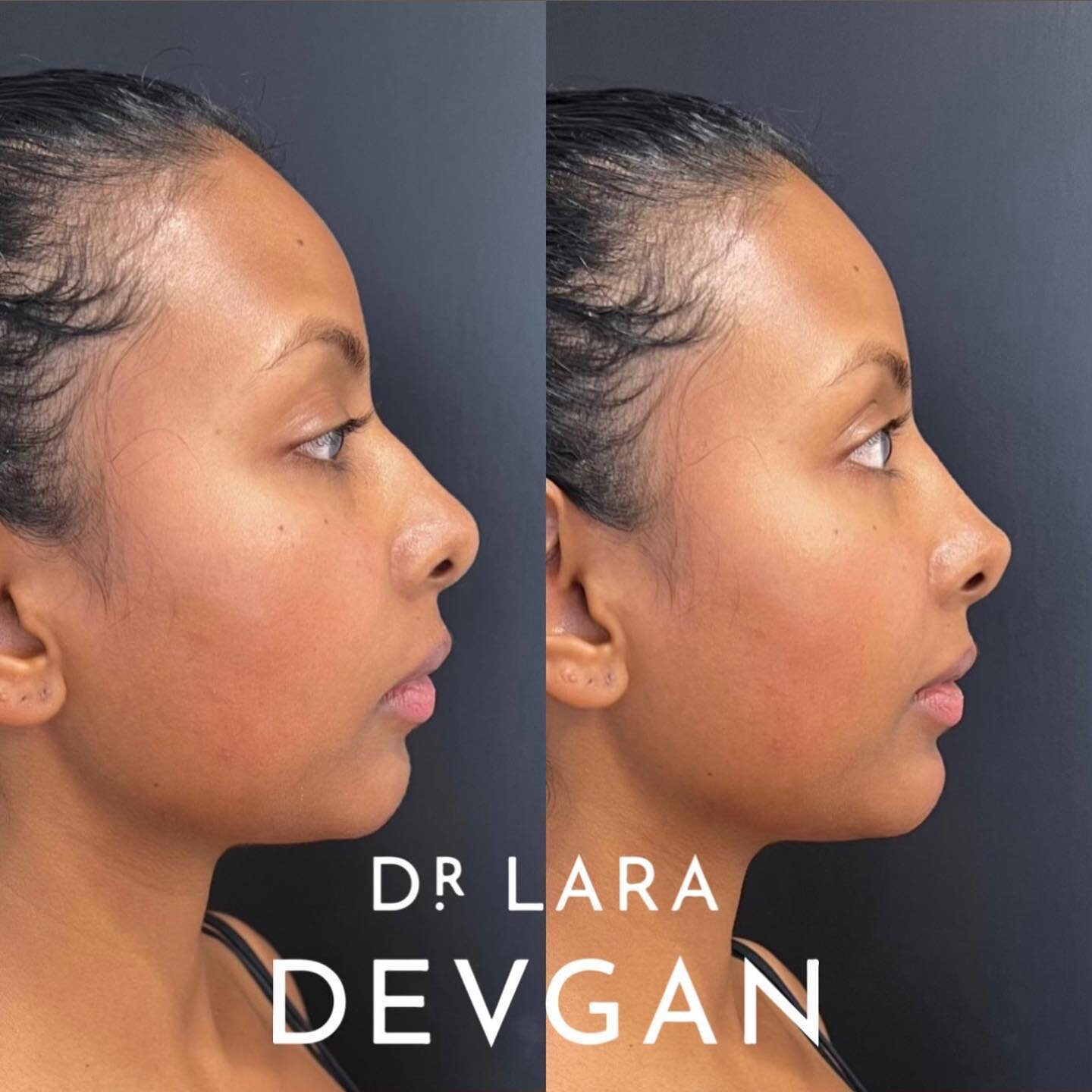
In select patients, fat grafting or hyaluronic acid filler (typically Juvederm or Restylane) can be used to fill in the tear troughs. For most, though, at this stage, surgical correction of aging eyes-- blepharoplasty or eye lift surgery-- comes into play.
Before considering blepharoplasty, a potential candidate must be appropriately medically cleared for the operation. This includes taking a detailed ophthalmologic history, including history of prior Lasik surgery, prior cataract surgery, use of eyeglasses or contact lenses, and history of dry eye.
Patients are advised to wait at least six months after ophthalmologic surgery before considering a cosmetic procedure to the periorbital area. Those with history of dry eye should be advised that their postoperative symptoms are likely to continue or possibly worsen in some cases.
Preoperative evaluation of a blepharoplasty patient should include an assessment of skin elasticity and tissue integrity around the eyes, presence of ptosis, lower lid laxity as assessed with a manual snapback test, dry eye as assessed with a Schirmer test, intact doll's eye reflex, and bony orbital anatomy.
Those with a negative vector, or an orbital rim that is recessed as compared to the globe, present more challenging cases. Those with ptosis will require a levator advancement or partial resection of conjunctiva and Muller's muscle to make the eyes appear symmetric postoperatively. Those with more than 6 mm of lower lid laxity will require a lid tightening maneuver such as a canthopexy or canthoplasty.
A cosmetically pleasing blepharoplasty requires a thorough understanding and appreciation of the complex anatomy around the eye. My preferred approach to an upper lid blepharoplasty involves the elevation of an elliptical or almond shaped skin-muscle flap, a conservative dissection of the medial and middle fat pads, and a possible pexy of a prolapsed lacrimal gland.
Incisions must be planned carefully so that they are hidden in the normal lid crease while at repose. Care must be taken to avoid overresecting the upper lid fat pads, as this can create a cadaveric appearance or so-called "A-frame" deformity. Care must also be taken to avoid damage to the lacrimal glands when performing any possible lifting or pexying maneuver.
My preferred approach to the lower lid blepharoplasty is via at a transconjuncival incision with modest to moderate resection of the three lower lid fat pads. Any excess skin can then be resected at the subciliary margin, using a conservative pinch test to determine the amount resected. In those patients with any degree of lower lid laxity, a canthopexy or canthoplasty will tighten the lower lid and decrease risk of postoperative lid malposition. Judicious repositioning of fat can assist with filling in a nasojugal or tear trough deformity.
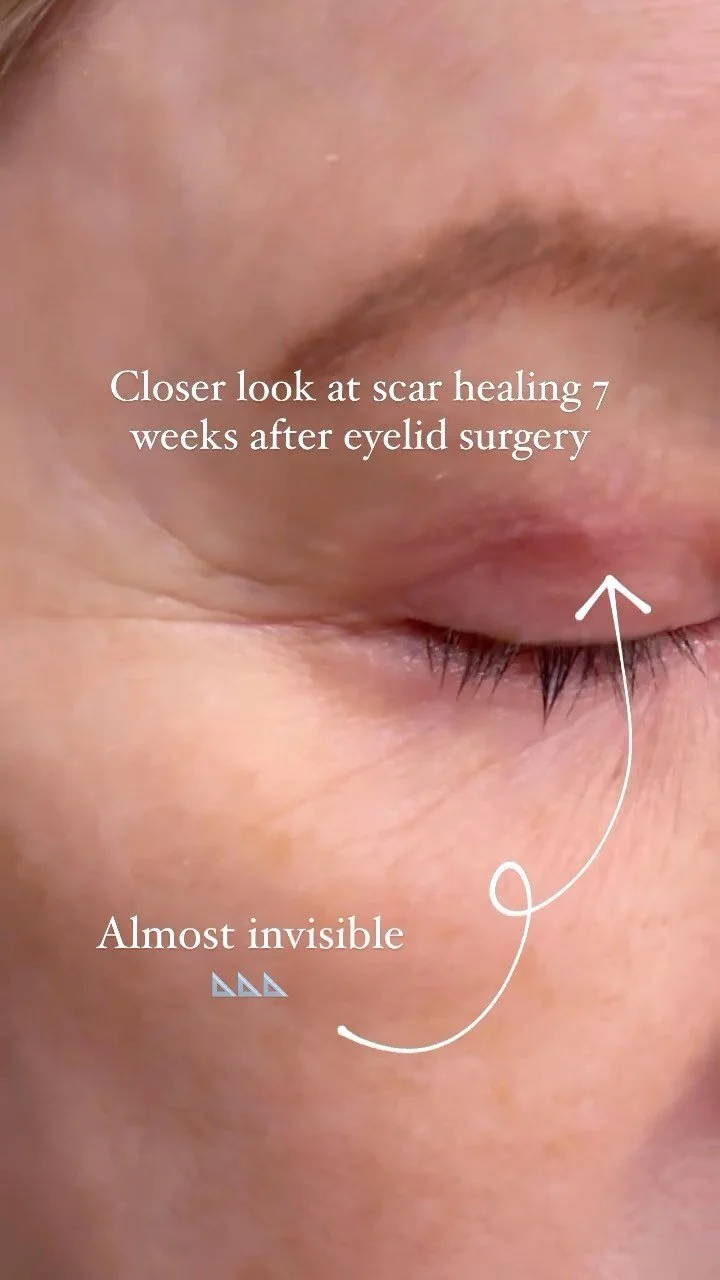
Postoperatively, patients are treated with ice packs, analgesia, and ophthalmic lubrication. Most are up and about on postoperative day one and back to work on postoperative day seven.
Postoperative results from upper and lower lid blepharoplasty are overwhelmingly positive. Patients report looking and feeling more awake, alert, youthful, and attractive. Indeed, when performed correctly, a 4-lid blepharoplasty can make appropriate surgical candidates look like a better version of themselves.
Blepharoplasty is not without its challenges, however. A rare but emergent complication of blepharoplasty is retrobulbar hematoma, which requires an immediate return to the operating room for evacuation and possible lateral canthotomy. A more frequent complication is lower lid malposition or ectropion. This is initially managed conservatively with massage, taping, and ophthalmic lubrication. If conservative management fails to resolve lower lid malposition within six months, the patient may require a return trip to the operating room for placement of a spacer graft, skin graft, and/ or lid tightening. Rarely a tarsal strip canthoplasty is required.
When it comes to periorbital aging, I advocate seeing a specialist who is capable of offering you each possibility in the treatment ladder. Whether you need skin care, injectable fillers, or surgery, you will be able to get properly assessed and treated. For questions about this article, please feel free to contact me directly via LaraDevganMD.com.